
England
The emergence of bacteria that cause infections in humans which are resistant to treatment with antibiotics has become a global public health concern.
Infections by multi-resistant germs are estimated to kill around 25,000 people in the EU every year, with some experts estimating that this number will increase dramatically over the coming decades.
But the situation between each member states varies hugely. Some countries have strict rules around antibiotic consumption and some don’t. The EU bodies responsible for addressing the problem recognise that there is no one-size-fits-all solution. This is why it is important to understand the situation in individual countries.
The issue in the UK
In the past few years, antibiotic resistance has become an increasingly prominent issue in British policy. In 2013 the government developed a five year cross-party strategy to combat antibiotic resistance. As part of this strategy, in 2014 the Prime Minister commissioned the leading economist Lord Jim O’Neill to chair the Review on Antimicrobial Resistance, a new initiative set up to analyse antibiotic resistance and come up with solutions to the problem.
Because of a series of MRSA outbreaks in the mid-2000s, there is a good awareness of the dangers of antibiotic resistance. The outbreaks reached a record high in 2006 when MRSA caused or contributed to 1,652 deaths. Since then there have been various directives on hygiene in hospitals and the number of deaths has fallen in recent years. In addition, the UK government has launched several awareness campaigns aimed at educating the public about the correct use of antibiotics.
MRSA prevalence
Percent of hospital Staphylococcus aureus isolates that are resistant to methicillin
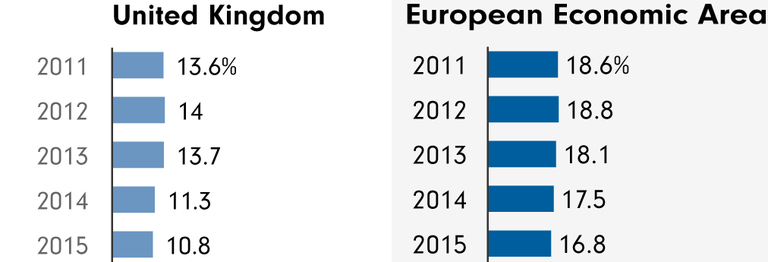
Source: ECDC
Data
Data on E. coli, C. difficile and MRSA infections is published by the government every year, month and quarter. However, there is no information on how many of these infections are resistant to some or all antibiotics.
The European Centre for Disease Prevention and Control (ECDC) regularly analyses data from participating hospitals. The data shows that the proportion of resistant forms of E. coli and S. aureus in the UK is low when compared to the European average.
The latest consumption data shows that 531.2 tonnes of antibiotics were given to humans, while livestock consumed 418.7 tonnes – this is around the European average.
Antibiotic consumption in humans
Daily doses per 1000 inhabitants per day
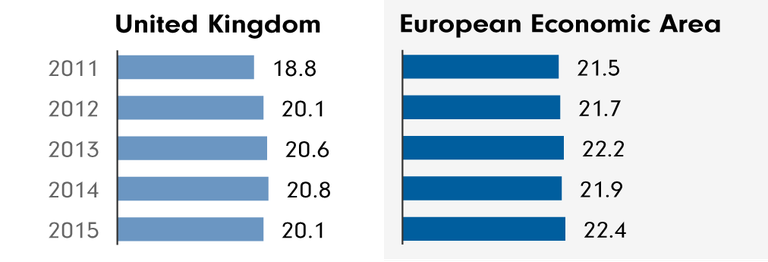
Source: ECDC
Hospital infections
An ECDC report which looked at infections and antibiotic use in European hospitals in 2011-12 reported on hospitals indicators like the use of alcohol hand rub and the number of single beds.
These indicators are important because they are measures that help to keep the rate of hospital acquired infections low, which helps to counter resistance – because the fewer infections patients acquire, the fewer antibiotics are used, and the less resistance can develop.
Single rooms are important because they can be used to isolate patients who have infections, preventing the infection from spreading. The amount of alcohol hand rub used indicates how well hospital staff are disinfecting their hands and following hygiene procedures – the more hand rub used, the less chance infections have of spreading.
England had a median alcohol hand rub consumption (in litres per 1,000 patient-days) of 25.3, almost the same as the European average of 25.64. However, hospitals in Northern Ireland only used 11.71 litres of alcohol hand rub per 1,000 patient-days, less than half the EU average.
The proportion of single room beds in hospitals across the UK was high compared to other European countries, from a median percentage of 27.06 single room beds among the total number of hospital beds in Northern Ireland, to 21.05 in Wales. The European average was 15.29 per cent single room hospital beds.
The ECDC report also looked at the number of doctors and nurses dedicated to infection prevention and control in each hospital. Scotland had the highest number of infection prevention and control nurses per 250 hospital beds in all of Europe, with a median of 2.14. This was also high across the rest of the UK, and well above the European average of 0.97.
The number of full time doctors dedicated to infection prevention and control varied across the UK. England was above the European average of 0.38 with 0.62 full time infection doctors per 250 hospital beds. Northern Ireland was well below the average with 0.23 full time infection doctors per 250 hospital beds. Data was not recorded for Wales or Scotland.
The ECDC also records HAI prevalence in European hospitals. This data shows what percentage of hospital patients have a hospital acquired infection – a large proportion of these infections are preventable, and are caused by poor hygiene.
The European average for HAI prevalence was 6.12%. In the UK, this number was around average at 6%.
-

-
Seven things YOU can do to combat antibiotic resistance
Because we can all help in the fight against resistant bugs.
-

A new TV documentary reveals that superbugs are multiplying in the polluted wastewater flowing from pharmaceutical plants in India
-

Less than half of antibiotics used in hospitals worldwide are prescribed appropriately, confirms a comprehensive new study
-

Projected death toll from drug-resistant superbugs 'based on incomplete data and flawed assumptions'
-

More antibiotics, more resistant germs
Antibiotic consumpion varies largely between countries
-

Antibiotics in the water
In India, high levels of antibiotic resistant germs have yet again been found in the water close to pharmacological plants
-

Lost life
More than two million Europeans are infected in hospital every year, according to the most comprehensive study to date
-

Top Priority Antibiotic Resistance
England has made antibiotic resistance a central issue in politics.
-

Fear of Bacteria
Why resistances against antibiotics has rather become an overestimated than an underestimated problem.
