Poland
The emergence of bacteria that cause infections in humans which are resistant to treatment with antibiotics has become a global public health concern.
Infections by multi-resistant germs are estimated to kill around 25,000 people in the EU every year, with some experts estimating that this number will increase dramatically over the coming decades.
MRSA prevalence
Percent of hospital Staphylococcus aureus isolates that are resistant to methicillin
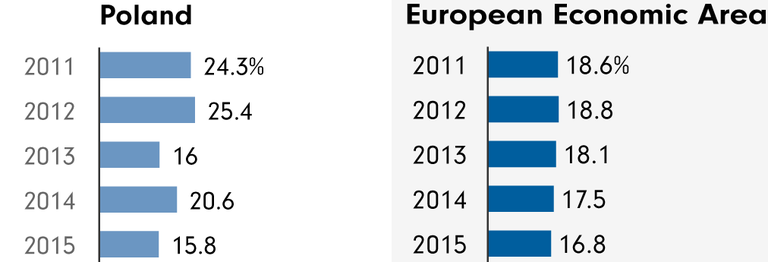
Source: ECDC
But the situation between each member states varies hugely. Some countries have strict rules around antibiotic consumption and some don’t. The EU bodies responsible for addressing the problem recognise that there is no one-size-fits-all solution. This is why it is important to understand the situation in individual countries.
In a major Eurobarometer survey on public attitudes to antibiotics, respondents were asked if they antibiotics were effective against a cough or a cold. Just over half of the respondents in the EU - 56 per cent - gave the correct answer, which is that antibiotics are not effective. But Poland was one of the countries, along with Greece and Bulgaria, where the public were least likely to answer this question correctly - only 34 per cent of respondents knew antibiotics wouldn’t cure a cough or cold.
Antibiotic consumption in Poland
In 2014, Poland collected data on antibiotic consumption in its hospitals for the first time. According to the European Centre for Disease Prevention and Control (ECDC), which published the data, 1.4 daily doses of antibiotics were taken per 1,000 people in Polish hospitals. This was lower than the EU average of 2.0 daily doses per 1,000 people.
Outside of hospitals, in 2014, 22.8 daily doses of antibiotics were taken per 1,000 people in Poland. This was just above the EU average of 21.6 daily doses per 1,000 people.
Antibiotic consumption in humans
Daily doses per 1000 inhabitants per day
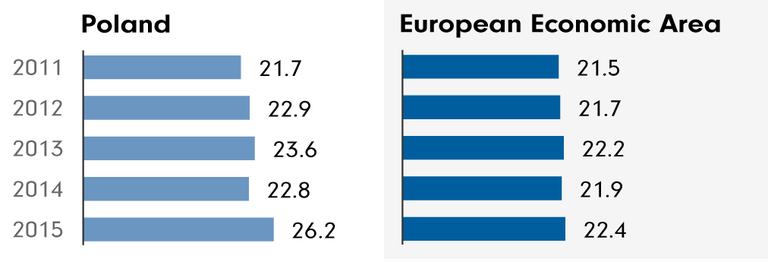
Source: ECDC
Hospital infections
The ECDC also records hospital associated infection (HAI) prevalence in European hospitals. This data shows what percentage of hospital patients have a hospital acquired infection – a large proportion of these infections are preventable, and are caused by poor hygiene.
The European average for HAI prevalence was 6.12%. In Poland, this number was around the average at 6.4%.
Livestock consumption of antibiotics
Poland is the leading EU producer of poultry meat, and in 2014 578.5 tonnes of antimicrobials were sold for use in livestock, the equivalent of 140.8 mg per PCU.
Between 2011 and 2014 this figure increased by 11 per cent, mainly because of an increase in the sales of penicillins and macrolides. Tetracyclines were the most-sold antibiotic in 2014 at 31 per cent of total sales.
Sales of critically important antibiotics for use in livestock also increased in Poland between 2011 and 2014, according to the EMA report. 3rd and 4th generation cephalosporin sales increased from 0.07 per cent to 0.12 per cent of total sales, but this was still below the EU average.
Fluoroquinolone sales also increased, from 5.7 per cent to 6.4 per cent of the total sales. In 2014, sales in mg/PCU of fluoroquinolones were 9.4, while the average across Europe was three times less at 2.99.
Other indicators
The ECDC reported on infections and antibiotic use in hospitals and included various indicators for hospitals across Europe in 2011-12, including the amount of alcohol hand rub used and the proportion of beds in single rooms.
These indicators are important because they are measures that help to keep the rate of hospital acquired infections low, which helps to counter resistance – because the fewer infections patients acquire, the fewer antibiotics are used, and the less resistance can develop.
Single rooms are important because they can be used to isolate patients who have infections, preventing the infection from spreading. The amount of alcohol hand rub used indicates how well hospital staff are disinfecting their hands and following hygiene procedures – the more hand rub used, the less chance infections have of spreading.
Polish hospitals only used on average 14.10 litres of alcohol hand rub per 1,000 patient days – much lower than the European average of 25.64.
Hospitals in Poland also had one of the lowest proportions of beds in single rooms, with just 3.42 per cent of hospital beds in a single room, compared to a European average of 15.29 per cent. Only Romania (2.93 per cent), Greece (2.86 per cent) and Hungary (1.71 per cent) had lower proportions of single room beds.
The report also looked at the number of doctors and nurses dedicated to infection prevention and control in each country. The European averages were 0.97 infection nurses per 250 hospital beds and 0.38 infection doctors per 250 beds. Poland was close to the average for both with 0.99 full time equivalent infection nurses per 250 beds, and 0.33 infection doctors per 250 beds.