E. coli – Cephalosporins
The WHO warns of Escherichia coli (E. coli) bacteria resistant to cephalosporin-antibiotics. Here you can see their prevalence in Europe’s hospitals. The percentage indicates the ratio of E. coli found to be resistant to this particular antibiotic.
The bug
Escherichia coli was named after the German pediatrician Theodor Escherich, who discovered the germ in 1885. Humans owe much to the bacterium, whether for its role in producing vitamins in our gut or as the subject of research that has helped solve many mysteries of molecular biology. But E. coli can play rough, too. When it gets into the wrong part of the body, it is one of the most common causes of harmful urinary tract and blood infections. It is also one of the leading causes of food infections. It is especially dangerous in hospital outbreaks. Some strains, like EHEC, can produce toxins and cause bloody diarrhea.
The resistance
Cephalosporins work on many different bacteria by inhibiting their reproduction. The first substance of this class was discovered in 1945 in mold. Cephalosporins have been chemically improved over time, so that they can also combat resistance. They are classified into generations. Third-generation cephalosporins are modern substances with a high relevance for battling hospital infections. Resistance is mainly caused by mechanism that degrade antibiotics.
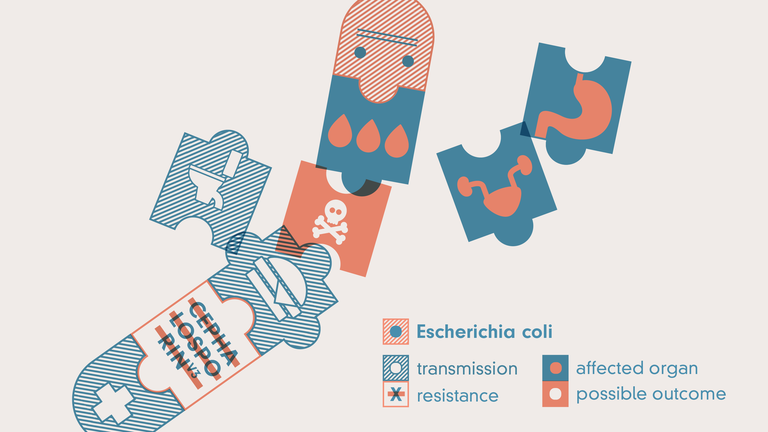
E. coli is transmitted through food and lacking hygiene. It is especially dangerous in hospitals, where it can infect the urinary tracts and blood of patients. Some strains can be dangerous in the gut, too. The worst possible outcome is death.
Text: Hristio Boytchev
Illustration: Nick Böse
Graphics: Simon Wörpel
Copy Editing: Christine Coester
